About
Alliance Secondary HealthWhat is Alliance?
Alliance Secondary Health is a product that complements a comprehensive major medical plan with a supplemental health insurance product that is administered by United Group Programs, Inc. under the brand name OptiMed. This product can be customized to work in conjunction with any primary health insurance provider in the marketplace. Alliance Secondary Health is not a replacement for your primary coverage, but rather a supplement to your primary carrier’s health plan. Simply put, Alliance Secondary Health pays the member’s portion of an eligible medical claim (i.e., copays, deductibles, and coinsurance) up to the annual maximum benefit. Benefits may be directed to the healthcare providers upon submission of the patient’s Itemized Bill or HCFA and the Primary Carrier’s EOB.
 Alliance Secondary Health is one of the few benefits that an employer can provide, which is universally beneficial. When implemented with the help of an Alliance consultant, your organization’s overall health insurance premiums should decrease and your employees will experience a reduction in their out-of-pocket expenses.
Alliance Secondary Health is one of the few benefits that an employer can provide, which is universally beneficial. When implemented with the help of an Alliance consultant, your organization’s overall health insurance premiums should decrease and your employees will experience a reduction in their out-of-pocket expenses.
The products offered by Alliance Secondary Health also provide numerous advantages by helping employers reduce single and family rates. Alliance is also helping employers achieve premium stability by allowing greater flexibility when picking a primary insurance plan design and by reducing the company’s claims experience with their primary provider.
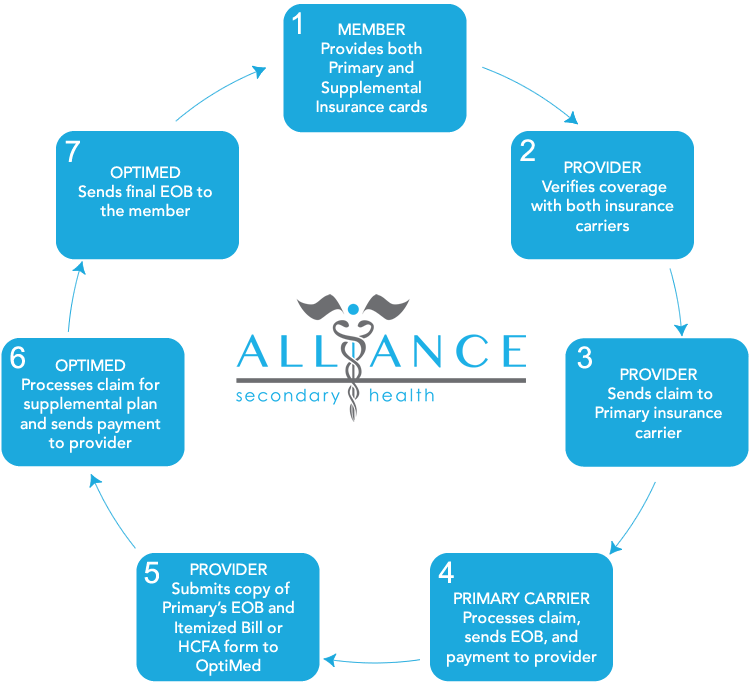
Provider Claims Process
With the Alliance Secondary Health product, healthcare providers can file patient claims via an electronic payer code that is clearly labeled on the member’s supplemental insurance card (note providers can also file via US mail). Here is how the claims process works:
Are you an individual needing to file a claim for reimbursement?
YES! How do I file a claim?
First, you need to obtain a copy of your Major Medical EOB (Explanation of Benefit) and Itemized Statement from your healthcare provider, showing procedures performed. The EOB can be found online via your primary insurance carrier’s portal or you will receive it via mail. The Itemized Statement (or HCFA) can be obtained from your physician’s office/hospital of care. You will also need to complete an OptiMed Claim Form with can be downloaded by clicking the button below.
Once you have obtained these items and completed the Claim Form you may file the claim to OptiMed via fax number (215) 968-6301 or you may submit the claim via US mail to:
OptiMed Health Plan
4 Terry Drive
Suite 1
Newtown, PA 18940
Alarming Healthcare Statistics
 Out-of-Pocket Costs
Out-of-Pocket Costs
Annual out-of-pocket responsibility for families covered by employer-sponsored health insurance in 2012 was $4,316. (Source: The 2012 Employer Health Benefits Survey, the Kaiser Family Foundation and the Health Research and Educational Trust (HRET), September 2012.)
Deductibles
- Nearly 30% of privately insured, working-age Americans with deductibles of at least 5% of their income had a medical problem but didn’t go to the doctor. Around the same percentage skipped doctor-recommended medical tests, treatments or follow-ups. (Source: USA Today, “Dilemma over deductible: Cost crippling middle class,” 2015)
- The percentage of covered workers in a plan with a deductible of at least $1,000 for single coverage grew from 31 percent to 34 percent in the past year. Covered workers in small firms remain more likely than covered workers in larger firms (49 percent vs. 26 percent) to be in plans with deductibles of at least $1,000. (Source: The 2012 Employer Health Benefits Survey, the Kaiser Family Foundation and the Health Research and Educational Trust (HRET), September 2014.)
Average Debt Recovery Rates
- Hospitals – 15.3 percent. (Source: ACA International’s Top Collection Markets Survey*, Jan. 1 – Dec. 2013.)
- Non-hospitals – 21.8 percent. (Source: ACA International’s Top Collection Markets Survey, Jan. 1 – Dec. 2013.)
Uncompensated Care/Bad Debt
U.S. hospitals provided $45.9 billion in uncompensated care in 2012, representing 6.1 percent of annual hospital expenses. (Source: American Hospital Association, “Uncompensated Hospital Care Cost Fact Sheet,” January 2014.)
The national average for bad debt is 5.93 percent, 3.03 percent for charity and 5.93 percent for total uncollectable accounts. The Midwest region of the U.S. had the highest percentage of total uncollectable accounts at 11.40 percent. (Source: The Hospital Accounts Report Analysis on Second Quarter 2014.)
Underinsured
As of 2012, 75 million people reported problems paying their medical bills or were paying off medical debt, up from 73 million in 2010 and 58 million in 2005. An estimated 48 million people were paying off medical debt in 2012, up from 44 million in 2010 and 37 million in 2005. (Source: Press release, The Commonwealth Fund, April 26, 2013.)
Premiums
In 2012, annual premiums for families covered by employer-sponsored health insurance averaged $15,745. Premiums rose 4 percent since 2011, but have risen 97 percent since 2002. (Source: The 2012 Employer Health Benefits Survey, the Kaiser Family Foundation and the Health Research and Educational Trust (HRET), September 2012.)
Cost of Care
In 2010, 41 percent of adults (ages 19-64) reported that they had medical debt or trouble paying medical bills, and 22 percent had been contacted by a collection agency for unpaid medical bills. (Source: The Commonwealth Fund Biennial Health Insurance Survey 2012, April 2013.)
Access to Care
In 2012, 43 percent of adults, or 80 million people, said they had skipped or delayed getting needed health care or filling prescriptions because of the cost. This is an increase from 75 million people who reported such problems in 2010, and 64 million in 2005. More than a quarter (28 percent) of adults with a chronic health condition said they had skipped doses or not filled a prescription for their health condition because of the cost. (Source: The Commonwealth Fund Biennial Health Insurance 2012, April 2013.)
Frequently Asked Questions
What is Alliance Secondary Health?
What is an eligible medical event?
Who files and pays the claims?
Is Alliance Secondary Health intended to replace my current health plan or provider?
Does Alliance Secondary Health have a restrictive network?
How is Alliance Secondary Health affected by the PPACA (||Obamacare||)?
Will Alliance Secondary Health increase the cost of our health insurance?
Are preexisting conditions excluded?
Who administers Alliance Secondary Health?
Alliance Secondary Health is administered by United Group Programs, Inc. under the brand name OptiMed. FSL has been rated A- (Excellent), based on an analysis of financial position and operating performance, by A.M. Best Company, and independent analyst of the insurance industry. For the latest rating, access www.ambest.com.
What is needed for an initial analysis?
(2) Current rates;
(3) Census of employees on your plan;
(4) Amount of HSA, HRA, or FSA employer contributions (if any);
(5) A meeting with an Alliance consultant.