Provider Services
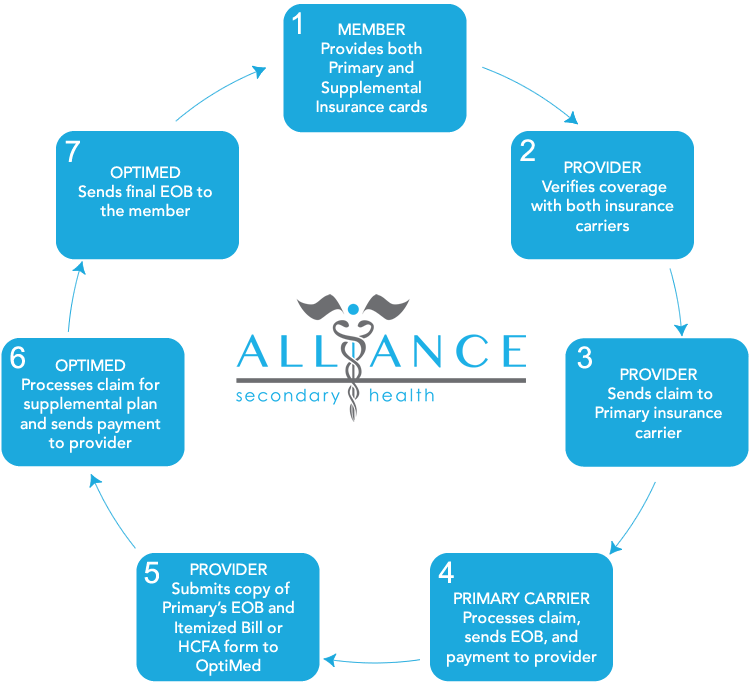
Alliance Secondary HealthClaims Filing
Provider Verifying Coverage
(800) 482-8770
US Mail Claims Submissions
OptiMed Health Plans
3145 Avalon Ridge PL Suite 300
Peachtree Corners, GA 30071-1543
EDI Claims Submissions
Clearing House: Change Healthcare
Payor ID: 96277
Phone Number: (800) 482-8770
Provider Filing Claims Must Include
- Itemized Bill or HCFA Form
- Copy of Primary Carrier EOB
Provider Portal
Click the button below to access or register to the provider portal:

Benefits to Providers
For services eligible under the patients’ primary health insurance, the Alliance Secondary Health plan administrator, United Group Programs, processes the claims for the patients’ out-of-pocket expenses such as copays, deductibles, and coinsurance. Claims are paid directly to the healthcare provider (unless the insured elects to not assign benefits to the provider). Alliance Secondary Health can offer many benefits to healthcare providers such as, but not limited to:
- Timely direct deposit payments.
- Reduction in Accounts Receivable.
- Reduction in the volume patient services that are delayed or avoided.
- Reduction in bad debt.
- Increase in patient utilization.
- Improvement in patient’s physical and financial wellbeing.
Frequently Asked Questions
How do I file a claim?
Electronic filings are made to OptiMed with clearing house Smart Data Solutions Payor ID# UGP19 and mailed claims are made to OptiMed Health Plans; 4 Terry Drive, Suite 1; Newtown, PA 18940. With all available methods, healthcare providers must include a copy of the Primary Carrier EOB and Itemized Statement or HCFA.